I have this format of the dataset in a text file.
Here the dataset link is https://drive.google.com/file/d/1RqU2s0dqjd60dcYlxEJ8vnw9_z2fWixd/view?usp=sharing
PMID- 20301691
STAT- Publisher
DA - 20100320
DRDT- 20210311
CTDT- 20000204
PB - University of Washington, Seattle
DP - 1993
TI - Classic Galactosemia and Clinical Variant Galactosemia
BTI - GeneReviews((R))
AB - CLINICAL CHARACTERISTICS: The term "galactosemia" refers to disorders of
galactose metabolism that include classic galactosemia, clinical variant
galactosemia, and biochemical variant galactosemia (not covered in this chapter).
This GeneReview focuses on: Classic galactosemia, which can result in
life-threatening complications including feeding problems, failure to thrive,
hepatocellular damage, bleeding, and E coli sepsis in untreated infants. If a
lactose-restricted diet is provided during the first ten days of life, the
neonatal signs usually quickly resolve and the complications of liver failure,
sepsis, and neonatal death are prevented; however, despite adequate treatment
from an early age, children with classic galactosemia remain at increased risk
for developmental delays, speech problems (termed childhood apraxia of speech and
dysarthria), and abnormalities of motor function. Almost all females with classic
galactosemia manifest hypergonadatropic hypogonadism or premature ovarian
insufficiency (POI). Clinical variant galactosemia, which can result in
life-threatening complications including feeding problems, failure to thrive,
hepatocellular damage including cirrhosis, and bleeding in untreated infants.
This is exemplified by the disease that occurs in African Americans and native
Africans in South Africa. Persons with clinical variant galactosemia may be
missed with newborn screening as the hypergalactosemia is not as marked as in
classic galactosemia and breath testing is normal. If a lactose-restricted diet
is provided during the first ten days of life, the severe acute neonatal
complications are usually prevented. African Americans with clinical variant
galactosemia and adequate early treatment do not appear to be at risk for
long-term complications, including POI. DIAGNOSIS/TESTING: The diagnosis of
classic galactosemia and clinical variant galactosemia is established by
detection of elevated erythrocyte galactose-1-phosphate concentration, reduced
erythrocyte galactose-1-phosphate uridylyltranserase (GALT) enzyme activity,
and/or biallelic pathogenic variants in GALT. In classic galactosemia,
erythrocyte galactose-1-phosphate is usually >10 mg/dL and erythrocyte GALT
enzyme activity is absent or barely detectable. In clinical variant galactosemia,
erythrocyte GALT enzyme activity is close to or above 1% of control values but
probably never >10%-15%. However, in African Americans with clinical variant
galactosemia, the erythrocyte GALT enzyme activity may be absent or barely
detectable but is often much higher in liver and in intestinal tissue (e.g., 10%
of control values). Virtually 100% of infants with classic galactosemia or
clinical variant galactosemia can be detected in newborn screening programs that
include testing for galactosemia in their panel. However, infants with clinical
variant galactosemia may be missed if the program only measures blood total
galactose level and not erythrocyte GALT enzyme activity. MANAGEMENT: Treatment
of manifestations: Standard of care in any newborn who is "screen-positive" for
galactosemia is immediate dietary intervention while diagnostic testing is under
way. Once a diagnosis is confirmed, restriction of galactose intake is continued
and all milk products are replaced with lactose-free formulas (e.g., Isomil((R))
or Prosobee((R))) containing non-galactose carbohydrates; dietary restrictions on
all lactose-containing foods and other dairy products should continue throughout
life, although management of the diet becomes less important after infancy and
early childhood. In rare instances, cataract surgery may be needed in the first
year of life. Childhood apraxia of speech and dysarthria require expert speech
therapy. Developmental assessment at age one year by a psychologist and/or
developmental pediatrician is recommended in order to formulate a treatment plan
with the speech therapist and treating physician. For school-age children, an
individual education plan and/or professional help with learning skills and
special classrooms as needed. Hormone replacement therapy as needed for delayed
pubertal development and/or primary or secondary amenorrhea. Stimulation with
follicle-stimulating hormone may be useful in producing ovulation in some women.
Prevention of secondary complications: Recommended calcium, vitamin D, and
vitamin K intake to help prevent decreased bone mineralization; standard
treatment for gastrointestinal dysfunction. Surveillance: Biochemical genetics
clinic visits every three months for the first year of life or as needed
depending on the nature of the potential acute complications; every six months
during the second year of life; yearly thereafter. Routine monitoring for: the
accumulation of toxic analytes (e.g., erythrocyte galactose-1-phosphate and
urinary galactitol); cataracts; speech and development; movement disorder; POI;
nutritional deficiency; and osteoporosis. Agents/circumstances to avoid: Breast
milk, proprietary infant formulas containing lactose, cow's milk, dairy products,
and casein or whey-containing foods; medications with lactose and galactose.
Evaluation of relatives at risk: To allow for earliest possible diagnosis and
treatment of at-risk sibs: Perform prenatal diagnosis when the GALT pathogenic
variants in the family are known; or If prenatal testing has not been performed,
test the newborn for either the family-specific GALT pathogenic variants or
erythrocyte GALT enzyme activity. Pregnancy management: Women with classic
galactosemia should maintain a lactose-restricted diet during pregnancy. GENETIC
COUNSELING: Classic galactosemia and clinical variant galactosemia are inherited
in an autosomal recessive manner. Couples who have had one affected child have a
25% chance of having an affected child in each subsequent pregnancy. Molecular
genetic carrier testing for at-risk sibs and prenatal testing for pregnancies at
increased risk are an option if the GALT pathogenic variants in the family are
known. If the GALT pathogenic variants in a family are not known, prenatal
testing can rely on assay of GALT enzyme activity in cultured amniotic fluid
cells.
CI - Copyright (c) 1993-2021, University of Washington, Seattle. GeneReviews is a
registered trademark of the University of Washington, Seattle. All rights
reserved.
FED - Adam, Margaret P
ED - Adam MP
FED - Ardinger, Holly H
ED - Ardinger HH
FED - Pagon, Roberta A
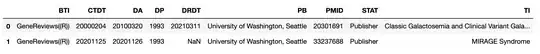
I want to give the left side value as column name and right side values will be a row format.
Output should be
PMID STAT DA CTDT
33237688 Publisher 20201126 20201125
I have tried with text to CSV but not working
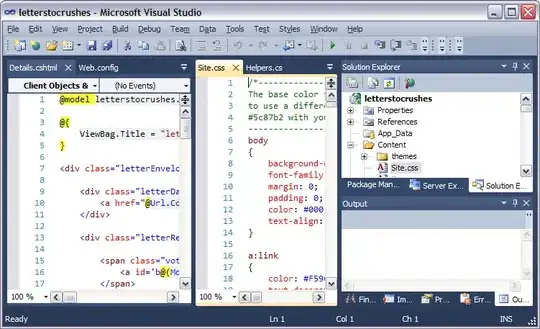
import pandas as pd
medical = pd.read_csv("sepsis2015.txt",
sep="\n")
print(medical)