This article was co-authored by Carrie Noriega, MD. Dr. Noriega is a Board Certified Obstetrician & Gynecologist and medical writer in Colorado. She specializes in women’s health, rheumatology, pulmonology, infectious disease, and gastroenterology. She received her MD from the Creighton School of Medicine in Omaha, Nebraska and completed her residency at the University of Missouri - Kansas City in 2005.
There are 15 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 25,128 times.
Postpartum bleeding, or lochia, is a natural although sometimes inconvenient part of recovery from childbirth, and it can last up to a month. The bleeding can be quite heavy in the first few days before tapering off significantly within the week. From there, it is usually more of a light period before reducing further to a light pink discharge (or 'spotting') within the month.[1] By taking care of yourself, taking preventative measures for leaking, and watching for symptoms of more serious conditions, you can make this time much easier to manage so you can focus on your baby.
Steps
Taking Care of Yourself
-
1Get plenty of rest. If you start bleeding bright red after having gotten past that state to pink or brown, you need more rest.[2] If you completely soak a pad within an hour, you should call a doctor. While the amount of rest you need will vary from person to person, increased bleeding or decreased mood suggests you should be getting more rest.[3] [4]
-
2Avoid sex for four to six weeks. The main reason for this is that because there are potential vaginal tears, as well as damage in the uterus, you can get an infection. It will also be uncomfortable immediately after birth to have sex, as you are likely to be sore.[5] You should wait until the bleeding is almost gone before having sex.[6]Advertisement
-
3Urinate frequently. You may not feel like you need to go, but keeping the bladder somewhat empty will help ease contractions. This will help to decrease pain and bleeding. You should call your doctor if you have the typical symptoms of a urinary tract infection, such as burning urination or a persistent urge to urinate.[7]
-
4Get plenty of iron. Iron is important because it helps to replenish your blood count after labor. You should try to get the iron you need from food sources, such as meats, beans and lentils, and certain vegetables such as broccoli or okra. This is because too much iron can cause constipation. You should only take an iron supplement if your doctor recommends it.[8]
Protecting Against Leaks
-
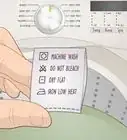
1Use pads, not tampons. Tampons can increase the chance of infection, and there are plenty of pads out there that can handle most flows.[9] [10] Consider using overnight or heavy flow pads, especially in the first week or so. You can even use pads regularly meant for urinary incontinence, as they tend to be bigger and more absorbent.[11]
-
2Wear disposable delivery underwear. These are mesh underwear that you can wear during the heavy period of postpartum bleeding. You will usually receive some pairs from the hospital. [12] However, you can buy them online as well. They are more convenient than traditional underwear, especially in the first few days after labor, when you’ll want to do nothing but rest.
-
3Invest in a waterproof mattress pad. This will help protect your mattress during sleep, and will give you some ease about leaks that can occur. If your flow is really heavy or you don’t want to stain your sheets, you might want to use a comfortable bed pad that rests on top of the sheets.[13]
-
4Keep a few disposable waterproof pads around the house. Using them when sitting on upholstered furniture, the carpet, or any other surface you want to protect from blood stains. These may not be necessary after the first week or so.[14] Using disposable pads are definitely more convenient, but you can use reusable ones if you want to be more environmentally friendly.[15]
Watching for Warning Signs
-
1Call a doctor if you pass blood clots bigger than golf balls. While some clots are normal, larger ones should raise concern. This can be a sign of postpartum hemorrhage, which can be fatal if left untreated. Other symptoms include pain in the vaginal region and low blood pressure.[16]
-
2Check your temperature if you feel feverish. If you have a fever of over 100.4 degrees, you should check with your doctor. It can be a sign of a serious infection. Fever with any of these other symptoms is especially concerning.[17]
-
3
-
4Watch the heaviness of the bleeding. If you are soaking a pad once an hour for more than two hours, you should call your doctor. It should be noted that normal moderate to heavy bleeding lasts for the first week or so. While the period may vary some, a return to very heavy bleeding should be looked into.[20]
-
5Count the weeks your postpartum bleeding continues. It should typically last two to six weeks. While it is normal for about 15% women to experience bleeding after six weeks, you will still want to talk to your doctor at your post-natal check, especially if the extended time occurs with any other symptoms.[21]
Warnings
- If you begin to feel unwell at any point, notice a strange smell, or are bleeding profusely, see a doctor immediately. It's always better to be safe than sorry.⧼thumbs_response⧽
- This information is not meant to replace medical advice.⧼thumbs_response⧽
References
- ↑ http://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/expert-blog/postpartum-bleeding/bgp-20055790
- ↑ http://www.nwh.org/community-health-resources/postpartum-guide/care-of-yourself/pain-management/#bleeding
- ↑ http://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/expert-blog/postpartum-bleeding/bgp-20055790
- ↑ https://www.nice.org.uk/guidance/ng194
- ↑ http://www.mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/postpartum-care/art-20047233?pg=2
- ↑ http://www.mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/postpartum-care/art-20047233
- ↑ http://www.mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/postpartum-care/art-20047233
- ↑ http://www.ghc.org/healthAndWellness/?item=/common/healthAndWellness/pregnancy/newMom/care.html
- ↑ http://www.nhs.uk/chq/Pages/2511.aspx?CategoryID=60
- ↑ http://www.webmd.com/parenting/baby/tc/postpartum-first-6-weeks-after-childbirth-recovery-at-home
- ↑ https://www.verywell.com/postpartum-bleeding-products-2759453
- ↑ http://nymag.com/thecut/2016/02/best-kept-secret-of-childbirth.html
- ↑ https://oasislactationservices.com/2013/06/04/5-things-you-actually-need-before-the-baby-comes/
- ↑ https://oasislactationservices.com/2013/06/04/5-things-you-actually-need-before-the-baby-comes/
- ↑ https://www.nsf.org/newsroom_pdf/BASF_Incontinence_Bed_Pads_EEA_Final_Oct2012.pdf
- ↑ https://www.uofmhealth.org/health-library/tn9119
- ↑ https://my.clevelandclinic.org/health/articles/9682-pregnancy-physical-changes-after-delivery
- ↑ https://www.merckmanuals.com/home/women-s-health-issues/postdelivery-period/postpartum-infections-of-the-uterus
- ↑ https://www.merckmanuals.com/home/women-s-health-issues/postdelivery-period/postpartum-infections-of-the-uterus
- ↑ https://my.clevelandclinic.org/health/articles/9682-pregnancy-physical-changes-after-delivery
- ↑ http://www.nwh.org/community-health-resources/postpartum-guide/care-of-yourself/pain-management/#bleeding

































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...